Setting A Gold Standard in Sepsis Care
LSU and Our Lady of the Lake Health Pioneer New Sepsis Test, Saving Lives, Cost
In hospitals nationwide, more people die from sepsis than from anything else. It’s more deadly than opioid overdoses, breast cancer and prostate cancer combined, and is the leading cause of hospital admission and readmission. It’s also one of the most difficult diseases to diagnose. But since August, a new sepsis test based on LSU and Our Lady of the Lake Health research and advances in microfluidics is saving lives and cost at Our Lady of the Lake Health in Baton Rouge, Louisiana.
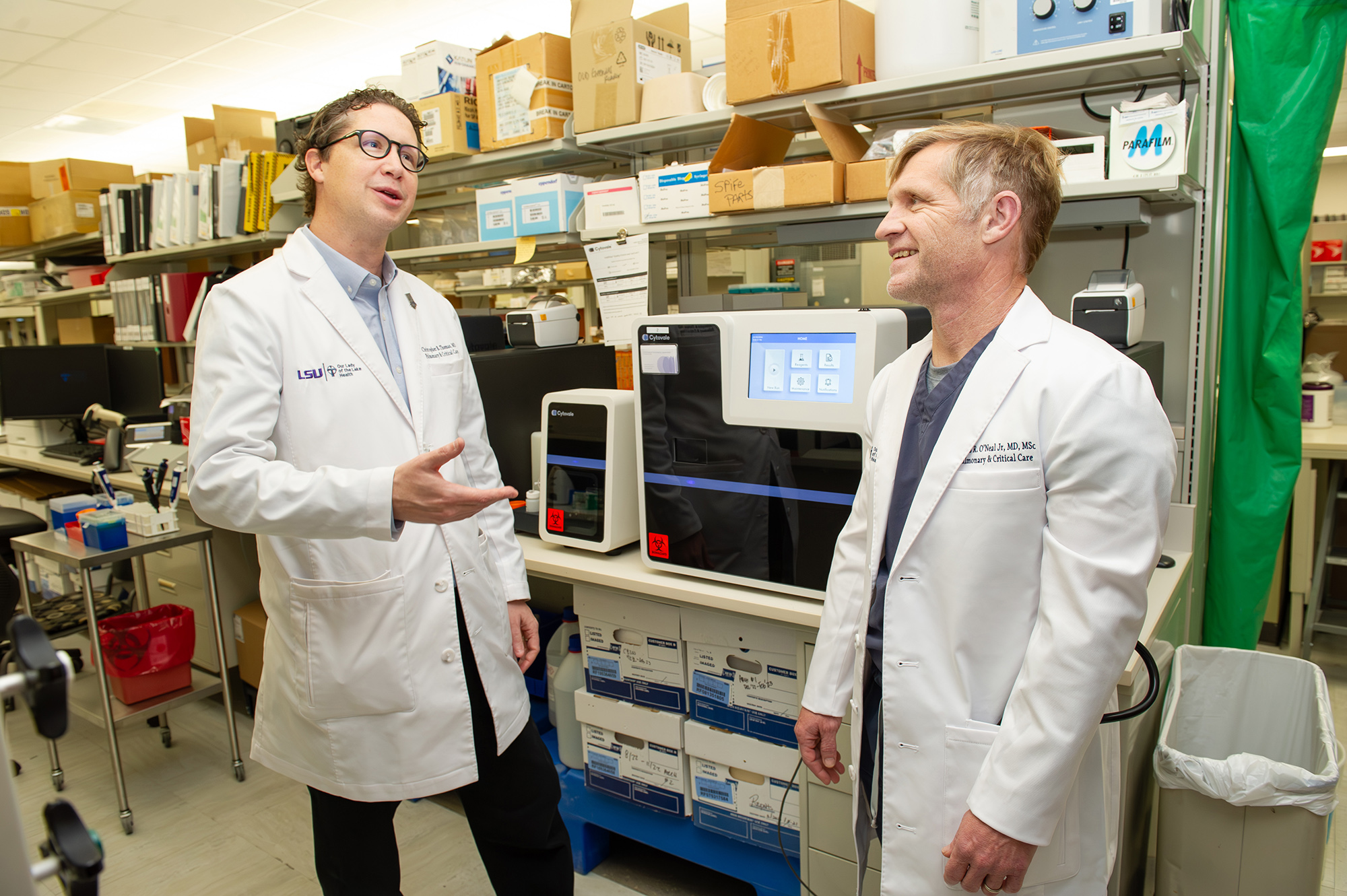
LSU Health New Orleans’ Dr. Bud O’Neal, who is from DeRidder, Louisiana, compares the new sepsis test he’s helped develop to a hurricane forecasting model. “You can drive around looking at the damage and say, ‘That was a hurricane,’ but that’s silly. You need to diagnose the hurricane when it’s still out in the Gulf, and we shouldn’t diagnose sepsis by looking at the damage that it caused.” On left, Dr. Christopher Thomas, vice president and chief quality officer for Franciscan Missionaries of Our Lady Health System and assistant professor of clinical medicine at LSU Health New Orleans, who has helped put the test into use at Our Lady of the Lake Health in Baton Rouge to save lives and cost for both patients and the hospital.
– Elsa Hahne/LSU
“We used to do the best we could,” said Dr. Christopher Thomas, chief quality officer for Franciscan Missionaries of Our Lady Health System, which operates six major medical centers in Louisiana and Mississippi, including Our Lady of the Lake Health in Baton Rouge. “Now, through translational research, we have a test that allows us to do personalized medicine that is improving our speed and efficacy. After six months, our results show that a higher percentage of patients are returning home to their families earlier, at lower cost for them and the hospital. Just our ability to improve patient flow has been revolutionary.”
Time is the primary challenge in sepsis care. Every hour that passes before a patient with sepsis receives treatment makes it eight percent more likely they’ll die. The life expectancy of people with untreated sepsis is three days or less. Meanwhile, early symptoms, such as chills, dizziness and a rapid heartbeat, could just as easily point to the flu or a panic attack.
“You come in with chest pain, we do an EKG; you have some weakness on the right side of your body, you go straight into what we call a stroke landing zone and get a CT scan,” said Dr. Thomas, who also serves as assistant professor of clinical medicine at LSU Health New Orleans. “But with sepsis, all we used to have—what every hospital in America currently has, except for Our Lady of the Lake—was a combination of vital signs that predicted something. So, we could treat you, perhaps unnecessarily, without being clinically sure, or wait until more tests and labs returned, which could mean extended time in the waiting room. This made our sepsis care inefficient. Now, we’re using the IntelliSep test and patient-centered questions we’ve learned from our research to triage efficiently and effectively. We’re getting to where we’re pulling people out of the waiting room 60 minutes faster.”

While the solution to sepsis is relatively accessible and affordable—antibiotics and fluids—figuring out who should or shouldn’t receive the treatment was subjective until LSU and Our Lady of the Lake Health collaborated with Cytovale to develop IntelliSep, a rapid test that received FDA approval in December 2022. It is now used daily at Our Lady of the Lake Health in Baton Rouge, helping to pull patients out of the waiting room 60 minutes faster.
– Illustration courtesy of Cytovale
Sepsis is an extreme overreaction to infection, where a person’s white blood cells start attacking vital organs. When LSU Health New Orleans physician Dr. Hollis “Bud” O’Neal, who also serves as medical director of research at Our Lady of the Lake Health, started work on a rapid test for sepsis in 2014, he didn’t know the now FDA-approved test would be in clinical practice just 10 years later. It took multiple research studies with thousands of patients enrolled across the country and a large, collaborative team effort to get there.
The sepsis test itself relies on research advances in microfluidics. “When the white blood cells become activated, they undergo structural changes,” Dr. O’Neal said. “They become squishy, for lack of a better word, and we use microfluidics—the study of fluids in very small volumes—to detect the change. That’s how the test works.”
It only takes one or two drops of blood to run the sepsis test. The results come back in less than 10 minutes and indicate a high, intermediate, or low probability of sepsis.
“Almost everyone who comes into the emergency room has blood drawn, and we can get what we need for the sepsis test from the same tube of blood we run a CBC on,” Dr. O’Neal said.
CBC stands for complete blood count. It’s a routine blood test used to look at overall health and find a wide range of conditions, including at annual checkups and in emergency rooms. When a person starts having sepsis, the change in their white blood cells occurs before there is any sign of organ damage, making early detection critical.
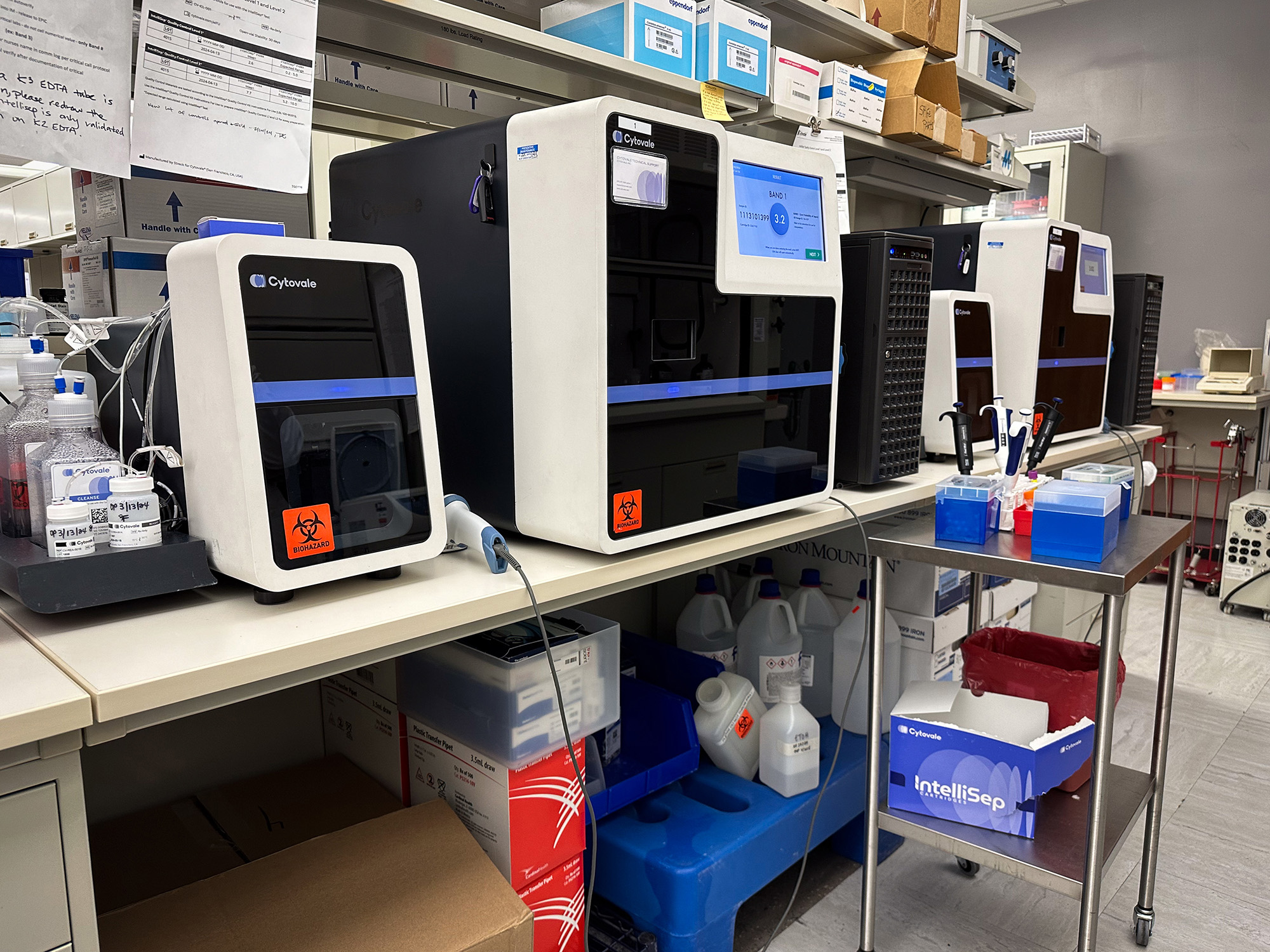
Our Lady of the Lake Health now has two Cytovale machines to run the sepsis tests. In 10 minutes or less, patients and providers can know if symptoms like chills, dizziness and a rapid heartbeat indicate life-threatening sepsis or perhaps instead flu or a panic attack.
– Elsa Hahne/LSU
While identifying patients with sepsis early is a big deal, identifying patients who don’t have sepsis is also important.
“Patients can be very sick, but if it’s something else that’s causing their illness, you can’t stick with sepsis, or odds are you’re going to miss something,” Dr. O’Neal said. “Our Lady of the Lake Health is now able to detect sepsis earlier in patients in whom it wasn’t really suspected, and get patients who don’t have sepsis quicker diagnosis and treatment. Overall, we’re saving patients more than a full day in the hospital.”
Dr. O’Neal hopes rural and critical access hospitals in Louisiana and elsewhere will be able to use the test soon.
“I’m from a small town—DeRidder, Louisiana—and one of the things I’m most interested in is helping to deliver better care in rural areas and at smaller hospitals,” Dr. O’Neal said. “They tend to be underserved and understaffed, and this technology could really help improve their sepsis care.”
Developing a test that receives FDA approval is one thing, while using that test in a hospital setting is entirely another, however, said Dr. Thomas:
“To deliver sepsis care at a world-class level, we need consistency and repeatability—we need process and continuous learning,” he said. “We’ve already changed the nurses’ workflow and taken what’s traditionally called a passive best-practice advisory and turned it into an active screen that requires an answer. Essentially, we’re saying to our teams that sepsis is just as critical as trauma, stroke and heart attacks. We need everyone to start a standard process as early as possible using the test. If action isn’t taken when it looks like it should have been, we now go and ask that triage nurse expert—what was it that made you dismiss the alert? All in order to learn and improve.”
While we’ve had the privilege of interacting with a number of universities, what’s been really special about the work with Dr. O’Neal and LSU has been their continuous focus on making sure the collaborative research and development we did together was always focused on patient needs. They’ve been the best partner we could have asked for.”
Ajay Shah, CEO of Cytovale, a medical diagnostics company that worked in concert with the team at LSU during the clinical development of the test
To ease broader implementation and make the test more useful, Dr. O’Neal’s team surveyed several hospitals and emergency departments.
“While most places have a process or plan of care for patients with possible sepsis, every site is different,” Dr. O’Neal said. “Some hospitals have a very nurse-driven process, while others have physician-driven processes. Some have processes they don’t follow, while others do, down to the comma. If we want our test to be used not just here at Our Lady of the Lake Health but at other hospitals, we have to help figure out how to integrate it into their workflows.”
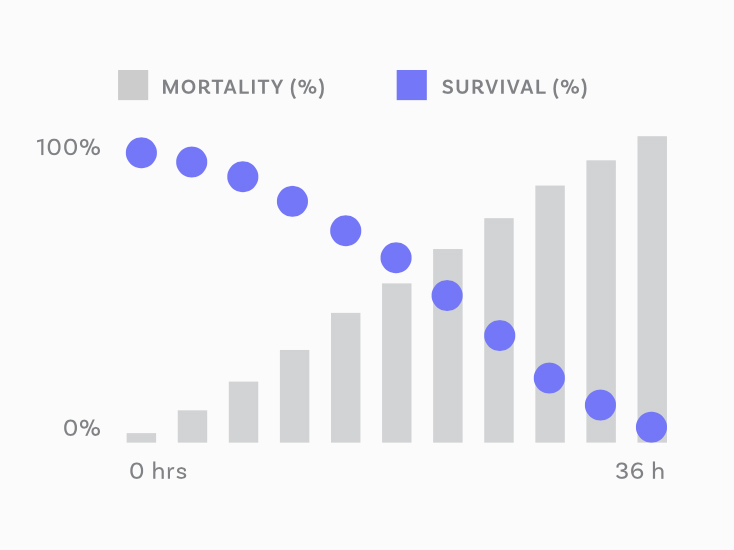
Since 2020, sepsis has led to about as many deaths as COVID-19. It’s a silent killer, and the leading cause of admission, readmission and death in hospitals. Every hour that passes before a patient with sepsis receives treatment makes it eight percent more likely they’ll die. The life expectancy of people with untreated sepsis is three days or less.
– Graph courtesy of Cytovale
The sepsis test was created by Cytovale, a medical diagnostics company that worked in concert with the team at LSU and Our Lady of the Lake Health during the clinical development of the test. Data has shown that up to 80 percent of sepsis deaths could be prevented with rapid diagnosis and treatment.
“While we’ve had the privilege of interacting with a number of universities, what’s been really special about the work with Dr. O’Neal and LSU has been their continuous focus on making sure the collaborative research and development we did together was always focused on patient needs,” said Ajay Shah, CEO of Cytovale, who received his PhD from the Harvard-MIT Division of Health Sciences and Technology. “They challenged us to develop this technology with the needs of emergency room patients first and foremost in our minds. They’ve been the best partner we could have asked for.”
To date, the ongoing collaboration between LSU, Our Lady of the Lake Health and Cytovale has enabled over 3,000 patients to be tested for sepsis at Our Lady of the Lake Health since the test was implemented in August 2023.
“We’re humbled to be able to partner with LSU and Our Lady of the Lake Health as they continue to improve care delivery in their communities,” Shah said.
Read More
LSU Health Sciences Physician Lead Investigator on Groundbreaking Sepsis Test


